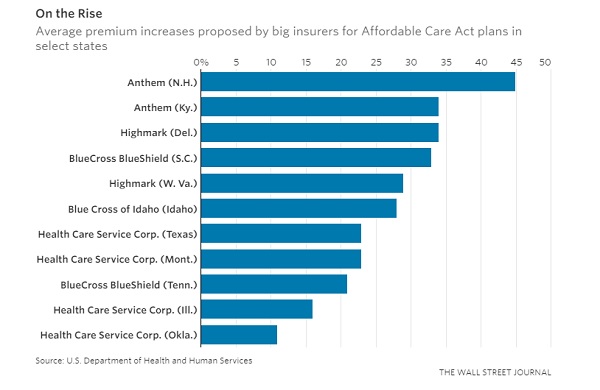
Major health insurers in some
states are seeking increases as high as 30% or more for premiums on 2018
Affordable Care Act plans, according to new federal data that provide the
broadest view so far of the turmoil across exchanges as companies try
to anticipate Trump administration policies.
Big insurers in Idaho, West
Virginia, South Carolina, Iowa and Wyoming are seeking to raise premiums by
averages close to 30% or more, according to preliminary rate requests published
Tuesday by the U.S. Department of Health and Human Services. Major
marketplace players in New Mexico, Tennessee, North Dakota and Hawaii indicated
they were looking for average increases of 20% or more.
In other cases, insurers are
looking for more limited premium increases for the suites of products they
offer in individual states, reflecting the variety of situations in different
markets. Health Care Service Corp., a huge exchange player in five states,
filed for average increases including 8.3% in Oklahoma, 23.6% in Texas, and 16%
in Illinois.
Together the filings show the
uncertainty in the health-insurance marketplaces as insurers around the U.S.
try to make decisions about rates and participation for next year amid open
questions about changes that could come from the Trump administration and
Congress.
Insurers face a mid-August
deadline for completing their rates. The companies have until late September to
sign federal agreements to offer plans in 2018. In some cases, insurers warn,
the figures revealed by federal regulators may not reflect their up-to-date
thinking.
The insurers’ decisions will be
closely dependent on moves by the Trump administration and Congress. Most
important is whether the federal government continues making payments that
reduce health-care costs for low-income exchange enrollees, which insurers say
are vital and President Donald Trump has threatened to halt.
Insurers are also concerned about
whether the Trump administration will enforce the requirement for most people
to have insurance coverage, which industry officials say helps hold down rates
by prodding young, healthy people to sign up for plans.
In Montana, Health Care Service
linked 17 percentage points of its 23% rate increase request to concerns about
the cost-sharing payments and enforcement of the mandate that requires everyone
to purchase insurance. Kurt Kossen, a senior vice president at Health Care
Service, said the company’s rate requests are driven by causes including
growing health costs and “uncertainty and the associated risks that exist
within this marketplace, including uncertainty around issues like the continued
funding of [cost-sharing payments] and mechanisms that encourage broad and
continuous coverage.”
Sen. Lamar Alexander (R., Tenn.),
who chairs the Senate committee that oversees health policy, said Tuesday that
he had told Mr. Trump directly that the government should continue making the
payments to insurance companies
The effect of the rate increases
will be blunted for many exchange enrollees, because lower-income people receive
federal subsidies that cover much of their premiums.
But increases could be tough to
stomach for those who aren’t eligible for the help, like Harland Stanley, 53,
of Louisville, Ky. Mr. Stanley, who owns his own research business, pays about
$400 a month for a plan from Anthem Inc., which is seeking an
average increase of 34% in the state, though Mr. Stanley’s own premiums might
rise by less or more than that.
“It’s going to hurt,” said Mr.
Stanley, who said his monthly premium this year is about $120 more than he paid
in 2016. “I worry about, what if it keeps going? When is this going to stop?”
Anthem, which is seeking rate
average increases of 30% or more in states including Colorado, Kentucky, Nevada
and Virginia, has said it would refile for bigger hikes and may pull back its
exchange offerings more if uncertainty continues around issues including the
cost-sharing payments.
Centene Corp.’s requests
ranged from less than 1% in New Hampshire to 21% in Texas and 12.49% in
Georgia. Those rate proposals generally assume the current rules surrounding
ACA plans continue, the company said.
Within the marketplaces, “there
is relative stability,” said Chief Executive Michael F. Neidorff. “The
uncertainty is driven by these policies on the ACA.”
CareSource, a nonprofit insurer
that offers exchange plans in four states, has prepared alternate rate filings
for different scenarios, and one of its state regulators Monday asked it to
refile with proposed rates that assume no cost-sharing payments.
“It’s challenging; you learn to
be very fluid,” said Steve Ringel, president of the Ohio market for CareSource.
According to actuarial firm Milliman Inc., at least seven states have made
similar requests in the past week, while others had earlier asked for two
versions of rate filings.
“Resolution of the [cost-sharing
payments] is an urgent issue,” said Bill Wehrle, a vice president at Kaiser
Permanente, which offers exchange plans in a number of states. “We’re coming up
at a point that’s fairly soon, where the pricing decisions we make are set for
all of next year.”
The impact of potentially losing
the cost-sharing payments was also clear in the rates requested by Blue Cross
of Idaho, which average 28%. That would probably be in the lower teens if the
payments were guaranteed, said Dave Jeppesen, a senior vice president. “It’s a
big swing,” he said. “There’s a lot of risk associated with the uncertainty in
Congress right now, and we are pricing appropriately for that risk.”
A recent Kaiser Family Foundation
analysis found insurers’ financial results on exchange plans improved in the
first quarter of this year, a sign of potentially emerging stability in the
business. That is reflected in a number of states where rate-increase requests
are limited. The exchange in California said Tuesday that insurers there were
seeking an overall average increase of 12.5%—but there would be an additional
12.4% boost layered onto middle-tier “silver” plans if the cost-sharing
subsidies aren’t paid.
However, in a number of cases,
insurers’ rate requests are well above 20% because of market factors not
directly tied to the federal uncertainty. Anthem has warned that it may need to
add 18% to 20% to its existing rate requests if the cost-sharing payments
aren’t locked in, and it may pull back in more states beyond the five exchanges
where it has disclosed plans to leave or sharply reduce its footprint. An
Anthem spokeswoman declined to comment on the company’s rate filings.
In Iowa, Medica said its rate
increase request was 43.5%, driven by the dynamics of the local market,
including the departure of other insurers and the fact that Medica itself has
been losing money because enrollees’ health costs ran higher than expected.
“You have some element of catching up to what the claims experience is,” says
Geoff Bartsh, a Medica vice president.
Medica’s requests in other states
have been far lower, he said, a sign of increased steadiness in those markets.
But, he said, if the cost-sharing payments go away, Medica estimates it will
need to add around 13% to 19% to its rate requests.
Click
here for the original article from Wall
Street Journal.